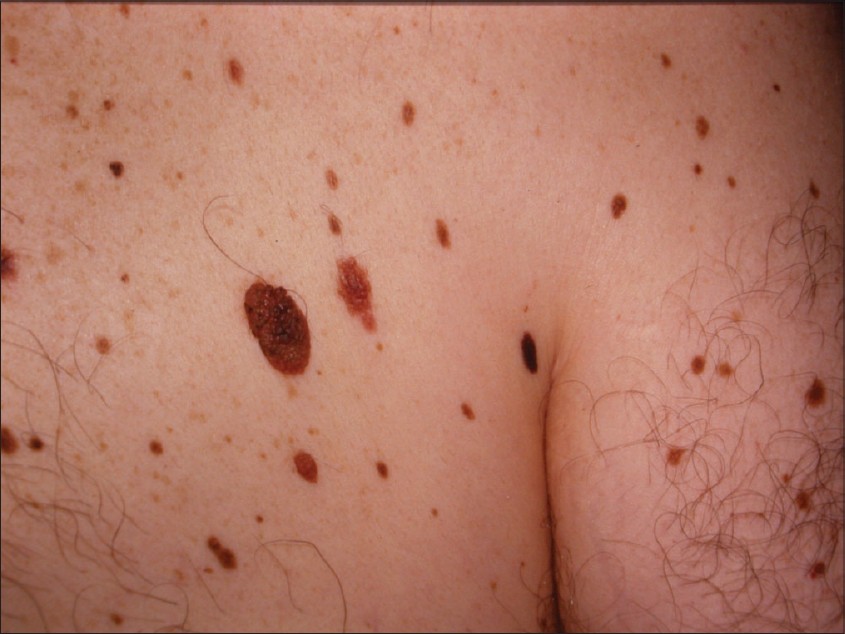
 Dysplastic Nevi (Atypical Moles) are unusual benign moles that may resemble melanoma. People who have them are at increased risk of developing single or multiple melanomas. The higher the number of these moles someone has, the higher the risk; those who have 10 or more have 12 times the risk of developing melanoma compared to the general population. Dysplastic nevi are found significantly more often in melanoma patients than in the general population.
Dysplastic Nevi (Atypical Moles) are unusual benign moles that may resemble melanoma. People who have them are at increased risk of developing single or multiple melanomas. The higher the number of these moles someone has, the higher the risk; those who have 10 or more have 12 times the risk of developing melanoma compared to the general population. Dysplastic nevi are found significantly more often in melanoma patients than in the general population.
Medical reports indicate that about 2 to 8 percent of the Caucasian population have these moles. Heredity appears to play a part in their formation.
Those who have dysplastic nevi plus a family history of melanoma (two or more close blood relatives with the disease) have an extremely high risk of developing melanoma. Individuals who have dysplastic nevi, but no family history of melanoma, still face a 7 to 27 times higher risk of developing melanoma compared to the general population–certainly a great enough risk to warrant monthly self-examination, regular professional skin exams and daily sun protection.
Normal Moles and Melanoma
Normal Moles are common small brown spots or growths on the skin that appear in the first few decades of life in almost everyone. They can be either flat or elevated and are generally round and regularly shaped. Many are caused by sun exposure.
Melanoma, one of the deadliest forms of skin cancer, most often appears as an asymmetrical, irregularly bordered, multicolored or tan/brown spot or growth that continues to increase in size over time. It may begin as a flat spot and become more elevated. In rare instances, it may not be pigmented.
“Classic" Atypical Mole Syndrome
Some people are so affected by both normal and atypical moles that they are classified as having atypical mole syndrome. They are at exceptionally high risk of developing melanoma. People with “classic” atypical mole syndrome have the following three characteristics:
- 100 or more moles
- One or more moles 8 mm (1/3 inch) or larger in diameter
- One or more moles which are atypical.
At exceptionally high risk of developing melanoma are those with familial atypical multiple mole melanoma syndrome (FAMMM). These individuals not only have atypical mole syndrome, but also have one or more firstor second-degree relatives with melanoma. While atypical moles often arise in childhood, they can appear at any time of life in people with FAMMM.
Warning Signs and Images
People with dysplastic nevi and a family history of dysplastic nevi and melanoma tend to develop the cancer at an earlier age than melanoma patients who don’t have such nevi. Individuals who have dysplastic nevi but no family history of dysplastic nevi and melanoma may also develop melanoma at a relatively early age, but less often.
At times it is difficult to distinguish between dysplastic nevi and early melanomas. (Sometimes, melanomas will begin within a dysplastic nevus.) To establish the difference, a doctor will remove the entire spot or a portion of it for examination in the pathology laboratory. Some physicians recommend examining the mole with a dermoscope, which magnifies and allows visualization of internal structures and colors not seen by the naked eye.
REMEMBER, ANY MOLE (PIGMENTED SPOT OR GROWTH) THAT UNDERGOES A SIGNIFICANT CHANGE IN SIZE, SHAPE, OR COLOR – OR THAT CAUSES SYMPTOMS OF ITCHING OR BLEEDING – SHOULD BE SUSPECTED OF BEING A MELANOMA.
Prevention Guidelines
Anyone who has an increased risk of developing melanoma must be particularly vigilant. Do any of these risk factors apply to you: light eyes, hair, and/or skin; freckles; many moles; personal or family history of melanoma or nonmelanoma skin cancer; sun sensitivity; inability to tan; repeated and intermittent sunburns; a very large mole present at birth, or dysplastic nevi?
The best advice is "Know your skin." Each family member should become aware of all moles on his/her total skin surface to minimize the risk of melanoma progressing to life-threatening stages. Anyone, especially someone with an increased risk of developing melanoma, should:
- Examine the skin completely each month, using a good light source (to illuminate the areas being examined), a full-length mirror and a hand-held mirror. Ask a family member or friend to help in examining hard-to-see parts of the body. A hair dryer is useful when checking the scalp. Also, examine the bottom of the feet and between the toes.
- Seek prompt medical attention if any of the warning signs of melanoma described earlier are found.
- Have a head-to-toe skin examination by a physician annually or more often. If moles are changing, as they may during adolescence, they should be checked at more frequent intervals. Inform your doctor about any moles that have suspicious signs, symptoms, or changes.
Suggestions for People with Dysplastic Nevi
If your doctor suspects dysplastic nevi, one or more moles may be biopsied - removed in a minor surgical procedure for microscopic examination. It is not necessary to remove all dysplastic nevi. However, if moles show significant change or signs of melanoma, or if new moles appear after age 40, they may be considered for removal by your physician.
When the diagnosis of dysplastic nevus is confirmed microscopically, it is advisable to:
- Write down a complete family history of unusual moles, melanomas or other cancers. Discuss it with your doctor.
- Have regular complete skin examinations at intervals suggested by your doctor, and advise family members to do the same.
- Supplement regular medical checkups with monthly self-examination of the skin.
- Reduce sun exposure. Excessive exposure may stimulate formation of new moles or even cause melanomas.
- Check with your doctor about having a set of full-body photographs taken, especially if family members have dysplastic nevi or melanoma and/or you have many moles. Changes can be more easily spotted in this way.
- Have any unusual or changing skin growth examined promptly by your doctor.
- Check with your physician to see if an eye examination is recommended, since moles and melanomas may also arise in the eyes.
- Be concerned, but don't worry excessively.
With regular self-examination, professional examination, and common sense, you greatly reduce your chances that a melanoma will grow to a threatening size before it can be detected and removed.
Preventing Skin Cancer
While skin cancers are almost always curable when detected and treated early, the surest line of defense is to prevent them in the first place. Here are some sun safety habits that should be part of everyone's daily health care:
- Seek the shade, especially between 10 AM and 4 PM.
- Do not burn.
- Avoid tanning and UV tanning booths.
- Cover up with clothing, including a broad-brimmed hat and UV-blocking sunglasses.
- Use a broad spectrum (UVA/UVB) sunscreen with an SPF of 15 or higher every day. For extended outdoor activity, use a water-resistant, broad spectrum (UVA/UVB)
 sunscreen with an SPF of 30 or higher.
sunscreen with an SPF of 30 or higher. - Apply 1 ounce (2 tablespoons) of sunscreen to your entire body 30 minutes before going outside. Reapply every two hours, or immediately after swimming or excessive sweating.
- Keep newborns out of the sun. Sunscreens should be used on babies over the age of six months.
- Examine your skin head-to-toe every month.
- See your physician every year for a professional skin exam.

